Papilloedema وذمة حليمة العصب البصري
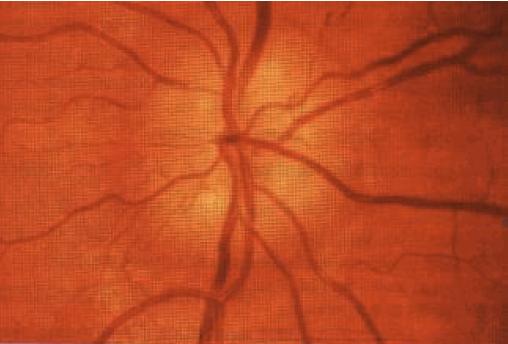
INSTRUCTION Examine this patient's fundus. SALIENT FEATURES History · Headache. · Transient visual disturbances. · Diplopia (due to associated sixth cranial nerve palsy). · History of hypertension, brain tumour. · History of ingestion of steroids, hypervitaminosis A (causes of benign intra-cranial hypertension). Examination · There is swelling of the optic disc (look for haemorrhages and soft exudates; Fig.78). Note. Remember that the common causes are: · Intracranial space-occupying lesion. · Hypertensive retinopathy. · Benign intracranial hypertension. DIAGNOSIS This patient has bilateral papilloedema (lesion) and I would like to investigate for an intracranial space-occupying lesion (aetiology). QUESTIONS What do you understand by the term 'papilloedema'? Papilloedema is the swelling of the nerve head as seen on ophthalmoscopy. The colour of the disc becomes redder, approximating to that of the rest of the retina; its contour becomes blurred and the cup and cribrosa are filled in. What is the first manifestation of papilloedema ? The earliest manifestation of papilloedema is the engorgement of the veins. What is the nature of the field defect in papilloedema? Papilloedema is always associated with enlargement of the blind spot with a con-sequent diminution of visual fields and gradual loss of visual acuity, but a fair degree of acuity may remain until papilloedema is marked. ADVANCED-LEVEL QUSTIONS : Mention a few causes of papilloedema. · Raised intracranial pressure resulting from one of the following conditions: - Impaired circulation of the CSF due to aqueduct stenosis. - Meningitis. - Subarachnoid haemorrhage. · Cerebral oedema: -Following head injury. -Following cerebral anoxia. · Metabolic causes: -Carbon dioxide retention. - Steroid withdrawal. -Thyroid eye disease. - Vitamin A intoxication. - Lead poisoning. · Increased protein in the CSF due to one of the following: - Guillain-Barre syndrome. -Spinal cord tumours. -Any spinal block. · Haematological and circulatory disorders: -Central retinal vein thrombosis. - Superior vena caval obstruction. - Polycythaemia vera. - Multiple myeloma. - Macroglobulinaemia. Mention a few conditions simulating papilloedema. · Deep optic cup: -Nasal edge appears heaped up. -Vessels plunge into the optic cup. -Temporal edge is quite normal. · Medullated nerve fibres, seen on the disc or even on the retina. The appearance is typically flared and on focusing will reveal fibres traversing the area. Field defects are due to the retinal vessels being obscured. Since these are present from birth. the patient is unaware of the defect. · Bergmeister's papilla, in which there is a whitish elevation of the centre of the disc with venous and arterial sheathing. It is common and seen at all ages. There is an equal sex and racial incidence. · Pseudopapilloedema, i.e. congenitally elevated discs secondary to hyaloid tissue (drtisen) or hyperopia. Note. Elevation or swelling of the optic disc occurs in the following conditions: · Papilloedema. · Papillitis. · Drtisen. · Infiltration of the nerve head by malignant cells. What do you know about Foster Kennedy syndrome? Unilateral papilloedema, with or without 'secondary' optic atrophy on the other side, suggests a tumour of the opposite side on the olfactory lobe or orbital surface of the frontal lobe or of the pituitary body. What do you understand by the term 'papillitis'? · Demyelination of the optic nerve (multiple sclerosis). · Inflammation. · Degeneration (Leber's optic atrophy). · Vascular disorders of the nerve head. · Malignant infiltration. How do you differentiate papillitis from papilloedema? Papillitis Papilloedema Usually unilateral Usually bilateral Visual acuity is considerably reduced Visual acuity only slightly reduced until in relation to the degree of swelling late stages of the disc Visual field defect is usually central, Peripheral constriction or enlargement particularly for red and green of the blind spot Marcus Gunn pupil may be present Marcus Gunn pupil is absent Eye movements may be painful Eye movements are never painful Note. A Marcus Gunn pupil is one that shows better constriction to an indirect response than to direct light. What are the stages of papilloedema ? · Stage I - increase in venous calibre and tortuosity. · Stage II - optic cup becomes pinker and less distinct, the vessels seeming to disappear suddenly on the surface of the disc. · Stage III - blurring of the discs on the nasal side. (Note. In many normal discs the nasal edge is less distinct and one of the most frequent false-positive signs is questionable blurring of the nasal disc margins.) · Stage IV - the whole disc becomes suffused and slightly elevated. The margins may disappear and the vessels seem to emerge from a mushy swelling. The optic cup is filled and there are haemorrhages around the disc. What are the features of benign intracranial hypertension? Dandy's diagnostic criteria (Brain 1991; 114:155-80): · Patient is alert. · Clinical features of increased intracranial pressure. · No localizing neurological signs (except sixth cranial nerve palsy). · Opening pressure of cerebrospinal fluid (CSF) during lumbar puncture is >20 cmH20 and CSF is of normal composition. · Normal ventricles and normal study on CT or MRI. What treatment options are available for pseudotumor cerebri? · Discontinuation of steroids, weight loss. · Drugs: carbonic anhydrase inhibitors, diuretics. · Serial lumbar punctures, lumboperitoneal shunt. · Optic nerve fenestration, subtemporal decompression. Foster Kennedy 0884-1952) was born in Belfast. He was Professor of Neurology at Cornell University. He described his syndrome in 1923.