Age-related macular degeneration (senile macular) تنكس اللطخة المتعلق بالتقدم بالعمر ( اللطخة الشيخية)
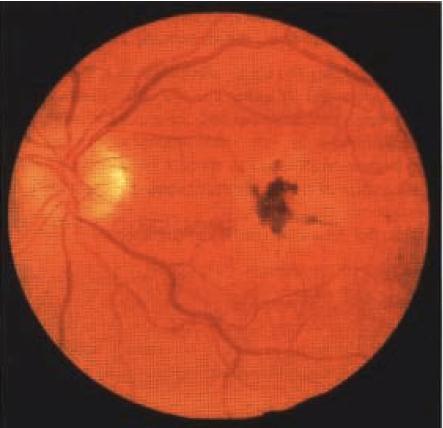
INSTRUCTION Look at this patient's fundus. SALIENT FEATURES History · Visual loss is often detected when one eye is covered for testing visual acuity. · Loss of ability to read, recognize faces or drive a car; however, patients have enough peripheral vision to walk unaided. · Decrease in visual acuity (severe loss suggests choroidal neovascularization). · Metamorphosia (distortion of the shape of objects in view). · Paracentral scotoma. · Variable visual loss due to atrophy of a large area of retinal pigment epithelium involving the fovea. · Family history. · History of smoking. · High blood pressure (increases risk of choroidal neovascularization). Examination · Drfisen. · Disruption of pigment of the retinal pigment epithelium into small areas of hypopigmentation and hyperpigmentation (Fig. 89). · Choroidal neovascularization. Proceed as follows: · Comment on the white walking aid by the bedside, which indicates the patient is registered blind. · Check visual acuity and visual field (in most patients there is loss of central vision and maintenance of peripheral vision). Patients with only driJsen typically require additional magnification of text and more intense light to read small print text. Remember that age-related macular degeneration is now the commonest cause of registrable blindness in the United Kingdom. DIAGNOSIS This patient has senile macular degeneration (aetiology) and is registered blind, as evidenced by the white walking aid (functional status). QUESTIONS What are drusen? Drusen are pale yellow spots that occur individually or in clusters throughout the macula. Nearly all individuals over the age of 50 years of age have at least one small drusen (?< 63 lam) in one or both eyes (Ophthalmology 1992; 14:130-42). They con-sist of amorphous material accumulated between Bruch's membrane and the pig-ment epithelium. Although the exact origin is not known, it is believed that driJsen occur due to the accumulation of lipofuscin and other cellular debris derived from cells of the retinal pigment epithelium that are compromised by age and other fac-tots. Only eyes with large dr0sen (>63 lam) are at increased risk for senile macular degeneration (Ophthalmology 1997; 104:7-21 ). What are the types of senile macular degeneration? There are two types: I. Atrophic or 'dry' type: involving the choriocapillaries, retinal pigment epithelium and the rods and cones. There is no leakage of blood or serum. 2. Neovascular exudative or 'wet' type: there is haemorrhagic or serous detachment of the retinal pigment epithelium and choroidal neovascularization resulting in leakage and fibrovascular scarring. ADVANCED-LEVEL QUESTIONS What do you know about neovascularization in these patients? Substantial visual loss occurs as a result of neovascularization. Choroidal vessels proliferate across Bruch's membrane under the retinal pigment epithelium and, in certain cases, continue their extension into the subretinal space. Substantial leakage from these neovascular membranes can result in retinal detachment. The most devastating consequence is haemorrhage, which resolves forming a disciform scar. What are the risk factors for choroidal neovascularization in the other eye of a patient with disorder in one eye? Large driJsen (>63 gm), more than 5 drtisen, focal hyperpigmentation of the retinal pigment epithelium. What investigations are performed to detect choroidal neovascularization ? · Rapid-sequence fluorescein angiography. · Retinal angiography using indocyanine green and infrared photography. How is the neovascularization treated? · Laser photocoagulation of regions outside the foveal avascular zone. · Subfoveal neovascularization: when photocoagulated is associated with a treatment-induced visual loss immediately but in the long term is found to be beneficial. Treatment may have to be deferred in those with good initial visual acuity because a large scotoma occurs as a result of treatment. · Photodynamic therapy with photosensitizers such as verteporfin is currently being evaluated. * Interferon-or is currently being evaluated. · Submacular surgery: surgical removal of subfoveal choroidal neovascularization has been reported to be useful but the results are not as good as laser photocoagulation. · Zinc: the use of zinc as a therapeutic agent for macular degeneration has not been evaluated in a rigorous trial. · External beam radiation therapy. · Thalidomide. · Others: indocyanine green-guided laser treatment, retinal transplantation and trans-plantation of retinal pigment epithelium, retinal translocation, retinal prosthesis, gene therapy. What is the difference between krypton and argon laser photocoagulation ? The krypton red photocoagulator is useful in treatment when the neovascularization is closer than 200 pm but not under the fovea, because of its ability to spare the inner retina by its virtual lack of absorption by haemoglobin (unlike the argon laser). The conventional argon laser has blue and green wavelengths. The green wave-length is absorbed by haemoglobin and thus may damage the retina, whilst the blue wavelength is absorbed by the macular xanthophyll and results in foveal damage. Mention some drugs that can cause maculopathy. Chloroquine, thioridazine, chlorpromazine.