Optic atrophy ضمور ( حثل ) العصب البصري
HTML clipboard
INSTRUCTION
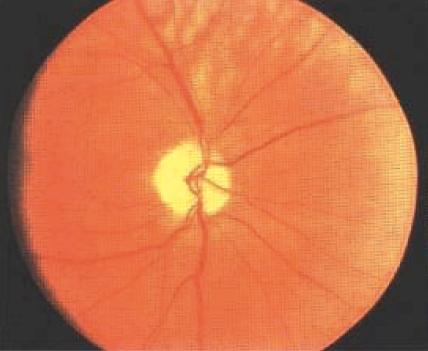
Examine this patient's eyes. Examine this patient's fundus. SALIENT FEATURES History Visual loss - onset of symptoms depends on underlying aetiology. History of multiple sclerosis. History of glaucoma. Optic nerve tumour. Vitamin B12 deficiency. Paget's disease. Exposure to toxins: lead, methanol, arsenic. Examination Pale disc with sharp margins Intact consensual light reflex but impaired direct light reflex - Marcus Gunn pupillary response (seen in asymmetrical involvement of the two eyes). Central scotoma on testing of visual fields. Proceed as follows: Tell the examiner that you would like to look for cerebellar signs (remember that multiple sclerosis is the commonest cause of optic atrophy). DIAGNOSIS This patient has primary optic atrophy (lesion) due to multiple sclerosis (aetiology). I would like to check the visual fields for central scotoma (functional status). QUESTIONS What is your diagnosis? The differential diagnosis is as follows: Demyelinating disorders (multiple sclerosis). Optic nerve compression by tumour or aneurysm. Glaucoma. Toxins: methanol, tobacco, lead, arsenical poisoning. Ischaemia, including central retinal artery occlusion due to thromboembolism, temporal arteritis, idiopathic acute ischaemic optic neuropathy, syphilis. Hereditary disorders: Friedreich's ataxia, Leber's optic atrophy (sex linked, seen in young males). Paget's disease. Vitamin B12 deficiency. Secondary to retinitis pigmentosa. ADVANCED-LEVEL QUESTIONS What is the difference between primary and secondary optic atrophy? Primary Secondary White and flat with clear-cut edges Greyish-white, edges indistinct Visible lamina cribrosa Cup filled and lamina cribrosa not visible Arteries and veins normal Arteries thinner than normal Veins may be.dilated Capillaries decreased in number Capillaries decreased in number (fewer than seven) - Kestenbaum's sign What is consecutive optic atrophy? Consecutive optic atrophy is a controversial term and is best avoided. Some use it as an equivalent or alternative for what has been described above as secondary optic atrophy, but others use the term to indicate an atrophy complicating retinitis or, rarely, Tay-Sachs disease or retinitis pigmentosa. What is glaucomatous optic atrophy? Glaucomatous optic atrophy denotes loss of disc substance, referred to as increased cupping. How would you investigate a patient with optic neuropathy? FBC, ESR. Blood glucose. Serology for syphilis. Vitamin Bi2 and B12 levels. Radiography of pituitary fossa, optic foramina and sinuses, or CT scan of the brain and orbit. ECG. Pattern-stimulated visual evoked responses. Electroretinography. R. Marcus Gunn (1850-1909), a Scottish ophthalmologist who worked at Moorfields Eye Hospital, London. T. von Leber (1840-1917), Professor of Ophthalmology at the University of Heidelberg, Germany. W. Tay (1843-1927), a British ophthalmologist, Moorfields Eye Hospital, London. B.R Sachs (1858-1944), a German neuropsychiatrist who worked in New York. He described this condition independent of Tay.