Mitral Regurgitation قصور الصمام التاجي ( القصور التاجي )
Mitral Regurgitation
INSTRUCTION
Examine this patient's heart.
SALIENT FEATURES
History
· Asymptomatic or mild symptoms: often. · Dyspnoea (due to pulmonary congestion). · Fatigue (due to
low cardiac output).
· Palpitation (due to atrial fibrillation or LV dysfunction).
· Fluid retention (in late-stage disease).
· Obtain a history of myocardial infarction, rheumatic fever, connective tissue dis-order, infective
endocarditis.
Examination
· Peripheral pulse may be normal or jerky (i.e. rapid upstroke with a short duration).
· Apex beat will be displaced downwards and outwards and will be forceful in character.
· First heart sound will be soft.
· Third heart sound is common (left ventricular gallop sound).
· Pansystolic murmur (Hope murmur) conducted to the axilla, best detected with the diaphragm and on
expiration. (Note. It is important to be sure that there is no associated tricuspid regurgitation.)
· Loud pulmonary second sound and left parasternal heave when there is associated pulmonary
hypertension.
Note. When mitral regurgitation is caused by left ventricular dilatation and dim-inished cardiac
contractility, the systolic murmur may be mid, late or pansystolic. Other causes of short systolic
murmurs at the apex include mitral valve prolapse, papillary muscle dysfunction and aortic stenosis. In
calcific aortic stenosis of the elderly, the murmur may be more prominent in the apex and may be
confused with mitral regurgitation. In such instances try to listen to the murmur after a pause with
pre-mature beat or listen to the beat after a pause with atrial fibrillation. The murmur of aortic stenosis
becomes louder, whereas that of mitral regurgitation shows little change.
DIAGNOSIS
This patient has mitral regurgitation (lesion) as evidenced by grade III/VI pan-systolic murmur, which is
probably due to ischaemic or rheumatic heart disease (aetiology), and is in cardiac failure as evidenced
by bibasal crackles (functional status). The patient is in NYHA class III heart failure.
QUESTIONS
Mention some causes of chronic mitral regurgitation.
· Mitral valve prolapse. · Infective endocarditis.
· Rheumatic heart disease. · Papillary muscle dysfunction.
· Left ventricular dilatation. · Cardiomyopathy.
· Coronary artery disease. · Connective tissue disorders.
· Annular calcification.
Mention a few causes of acute mitral regurgitation.
· Acute myocardial infarction (rupture of the papillary muscle).
· Endocarditis (due to perforation of the mitral valve leaflet or the chordae).
· Trauma.
· Myxomatous degeneration of the valve.
How would you investigate this patient?
· Electrocardiography (ECG), looking for broad bifid P waves (P mitrale), left ventricular hypertrophy,
atrial fibrillation. When coronary artery disease is the cause, there is often evidence of inferior or
posterior wall myocardial infarction.
· Chest radiograph, looking for pulmonary congestion, large heart, left atrial en-largement and
pulmonary artery enlargement (if severe and longstanding).
· Echocardiogram to determine the anatomy of the mitral valve apparatus, left atrial and left ventricular
size and function (typical features include large left atrium, large left ventricle, increased fractional
shortening, regurgitant jet on colour Doppler, leaflet prolapse, floppy valve or flail leaflet). The
echocardiogram provides baseline estimation of left ventricle and left atrial volume, an estimation of
left ventricular ejection fraction, and an approximation of the severity of regurgitation. It can be helpful
to determine the anatomic cause of MR. In the presence of even mild TR, an estimate of pulmonary
artery pressure can be obtained.
· Trans-oesophageal echocardiography is useful in those in whom transthoracic echocardiography
provides non-diagnostic images. It may give better visual-ization of mitral valve prolapse. It is useful
intraoperatively to establish the anatomic basis for MR and to guide repair.
· Cardiac catheterization is useful to determine coexistent coronary artery or aortic valve disease.
Large 'v' waves are seen in the wedge tracing. Left ventriculogram and haemodynamic
measurements are indicated when non-invasive tests are inconclusive regarding the severity of MR,
LV function, or the need for surgery.
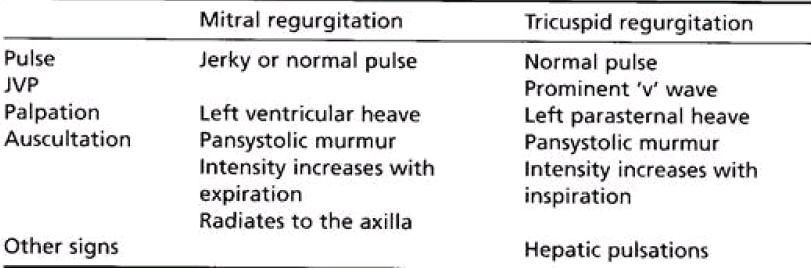
How would you differentiate between mitral regurgitation and tricuspid regurgitation ?
Why may these patients have a jerky pulse?
Because of reduced systolic ejection time, secondary to a large volume of blood regurgitating into the left
atrium.
When does the murmur of mitral regurgitation radiate to the neck (i.e. base of the heart)?
Rarely, due to involvement of the posterior mitral leaflet or to ruptured chordae tendineae, the regurgitant
jet strikes the left atrial wall adjacent to the aortic root and the murmur radiates to the base of the heart,
and therefore may be confused with the murmur of aortic stenosis.
How do you grade systolic murmurs?
Levine's grading of systolic murmurs (Ann Intern Med 1933; 6: 1371):
· Grade 1: Murmur is so faint that it is heard only with special effort.
· Grade 2: Murmur is faint but readily detected.
· Grade 3: Murmur is prominent but not loud.
· Grade 4: Murmur is loud.
· Grade 5: Murmur is very loud.
· Grade 6: Murmur is loud enough to be heard with the stethoscope just removed from contact with
the chest wall.
What are the causes of pansystolic murmur over the precordium?
· Mitral regurgitation.
· Tricuspid regurgitation.
· Ventricular septal defect (this generally radiates to the right of the sternum).
ADVANCED-LEVEL QUESTIONS
Which congenital cardiac conditions can be associated with mitral valve regurgitation ?
· Ostium primum atrial septal defect (due to cleft mitral valve).
· Partial atrioventricular canal.
· Corrected transposition of the great arteries.
How would you determine the severity of the lesion?
· The larger the left ventricle on clinical examination, the greater the severity.
· An S3 suggests that the disease is severe.
· Colour Doppler ultrasonography quantifies the severity of the regurgitant jet, usually into three
grades. However, echocardiography provides only a semi-quantitative estimate of the severity of
regurgitation. Left ventriculography performed during cardiac catheterization provides an additional
but also im-perfect estimate of the severity of mitral regurgitation.
· Prognosis is worsened if right ventricular function is reduced, and patients with a right ventricular
ejection fraction of <30% are particularly at high risk (Circulation 1986; 73: 900-12).
What is the significance of third heart sounds in mitral regurgitation?
The prevalence of third heart sounds increases with the severity of mitral regur-gitation. However, in
patients with mitral regurgitation, the third heart sound is due to rapid ventricular filling and does not
necessarily reflect left ventricular systolic
dysfunction or increased filling pressure. In this situation S3 is caused by rapid filling of the left ventricle
by the large volume et blood stored in the left atrium in diastole.
What is the medical management of such patients?
· Asymptomatic patients: antibiotic prophylaxis for endocarditis.
· When atrial fibrillation develops: digitalis to slow ventricular response.
· Heart failure: diuretics and inotropes, but major consideration should be given to surgery.
What are the indications for surgery in this patient?
· Moderate to severe symptoms despite medical therapy (NYHA functional class III or IV), provided
that left ventricular function is adequate.
· Patients with minimal or no symptoms should be followed up every 6 months by echocardiographic
or radionuclide assessment of left ventricular size and systolic function. When the ejection fraction
falls to 60% (Circulation 1994; 90: 830-7), or when left ventricular end-systolic dimension is greater
than 45 mm (JAm Coil Cardiol 1984; 3: 23542), mitral valve repair or replacement should be
con-sidered even in the absence of symptoms.
Remember that ischaemic mitral regurgitation carries the worse prognosis: operative mortality is 10-20%
and long-term survival is substantially lower than with non-ischaemic mitral regurgitation (J Thorac
Cardiovasc Surg 1986; 91: 379-88; Ann Thorac Surg 1994; 58: 668-75).
When is successful valve repair less likely?
It is less likely when the aetiology is ischaemic, infectious or rheumatic, when there is significant
calcification, when the prolapse is bileaflet or anterior.
What do you know about mitral regurgitation due to flail leaflet?
In patients with mitral regurgitation due to flail leaflet, the lesion usually results in high degrees of
regurgitation (J Am Coil Cardiol 1990; 16: 232-9). In Western countries flail leaflet is the most frequent
cause of mitral regurgitation requiring surgical correction (Mayo Clinic Proc 1987; 62: 22-34; Eur Heart J
1991; 12 suppl B: 2-4). When treated medically, mitral regurgitation due to flail leaflet is associated with
excess mortality and high morbidity. Surgery is almost unavoidable within 10 years after the diagnosis
and appears to be associated with an improved prog-nosis, suggesting that surgery should be considered
early in the course of the disease (N Engl J Med 1996; 335: 1417-23).
Samuel A. Levine was Professor of Cardiology at Harvard Medical School and Peter
Bent Brigham Hospital in Boston.
James Hope (1801-1841) was an English physician who worked at St George's Hospital, London, and
wrote a book in 1831 entitled Diseases of the Heart and Great Vessels.