Retinitis pigmentosa التهاب الشبكية الصباغية
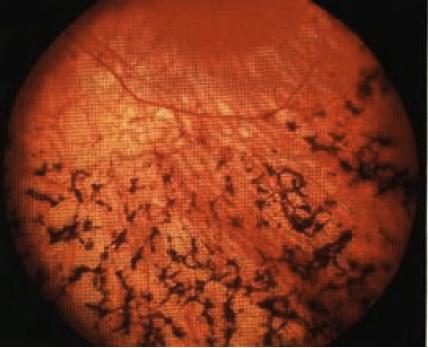
INSTRUCTION Examine this patient's fundus. Examine this patient's eyes. SALIENT FEATURES History · Family history of blindness (can be autosomal recessive, which is more severe, or autosomal dominant, which is more benign). · Decreased nocturnal vision. · Altered colour vision. · Loss of peripheral vision. · Blurry vision. Examination · Peripheral retina shows perivascular 'bone spicule pigmentation' and arteriolar narrowing (Fig. 82). The retinal veins (never the arteries) often have a sheath of pigmentation for part of their course. The pigment spots that lie near the retinal veins are seen to be anterior to them, so that they hide the course of the vessel. (In this respect they differ from the pigment around the spots of choroidal atrophy in which the retinal vessels can be traced over the spots.) span style='font-size:12.0pt;font-family:"Times New Roman";mso-fareast-font-family: "Times New Roman";mso-ansi-language:EN-US;mso-fareast-language:EN-US; mso-bidi-language:AR-SA'> · Optic disc is pale. · Maculopathy, which is atrophic or cystoid. Proceed as follows: · Look for polydactyly in the hands and feet (Laurence-Moon-Biedl syndrome). · Comment on the white walking aid (if any) used by the registered blind. · Tell the examiner that you would like to check visual fields. DIAGNOSIS This patient is obese, has polydactyly and retinitis pigmentosa (lesion) due to Laurence-Moon-Biedl syndrome (aetiology) and is registered blind (functional status). QUESTIONS What is the prognosis in retinitis pigmentosa? Most patients are registered blind by the age of 40 years, with central field less than 20° in diameter. Almost all patients lose central vision by the seventh decade. What do you know about retinitis pigmentosa? Retinitis pigmentosa is a slow degenerative disease of the retina. It occurs in both eyes, begins in early childhood, and often results in the loss of sight by middle or advanced age. The degeneration primarily affects the rods and cones, in particular the rods How may it present? It may present with defective vision at dusk (night blindness), which may occur several years before the pigment is visible in the retina. ADVANCED-LEVEL QUESTIONS Mention a few systemic disorders associated with retinitis pigmentosa. · Laurence-Moon-Biedl-Bardet syndrome, which is a recessively inherited dis-order characterized by mental disability, polydactyly, syndactyly, hypogonadism and obesity. · Bassen-Kornzweig syndrome (abetalipoproteinaemia), characterized by fat malabsorption, abetalipoproteinaemia, acanthocytosis and spinocerebellar ataxia (Ophthalmology 1984; 91: 991). · Refsum's disease (phytanic acid storage disease), an autosomal recessive disorder characterized by hypertrophic peripheral neuropathy, deafness, ichthyosis, cerebellar ataxia, raised CSF protein levels in the absence of pleocytosis. · Kearns-Sayre syndrome, a triad of retinitis pigmentosa, progressive external ophthalmoplegia and heart block (Br J Ophthalmol 1985; 69: 63). · Usher's disease, a recessively inherited disorder characterized by congenital, non-progressive, sensorineural deafness (Arch Ophthalmol 1983; 101:1367). · Friedreich's ataxia (see pp 191-3). Which ocular conditions are associated with retinitis pigmentosa? · Open-angle glaucoma. · Myopia. · Posterior subcapsular cataracts. · Keratoconus. What is secondary retinitis pigmentosa? Secondary retinitis pigmentosa is a sequela to inflammatory retinitis. It is often ophthalmoscopically indistinguishable from the primary condition; the electro-retinographic and electro-oculographic responses are slightly subnormal unless the condition is far advanced. (In the primary type the response is markedly subnormal to the electroretinogram and electro-oculogram). What is retinitis pigmentosa sine pigmento? A variety of retinitis pigmentosa without visible pigmentation of the retina. p class=MsoNormal style='text-align:left;mso-pagination:none;mso-layout-grid-align: none;text-autospace:none;direction:ltr;unicode-bidi:embed'>What is inverse retinitis pigmentosa? Bone corpuscles are visible in the perifoveal area, whereas the retinal periphery is normal. How would you manage this patient? · Refer for genetic counselling. · Impaired vision training and aids for daily living. · Refer for job training. · Regular ophthalmology follow-up including visual fields, electroretinogram. J.Z. Laurence (1830-1874), an English ophthalmologist. R.C. Moon (1844-1914), a US ophthalmologist. A. Biedl (1869-1933), a Czech physician. G. Bardet (b. 1885), a French physician. RA. Bassen (b. 1903), physician, and A.L. Kornzweig (b. 1900), ophthalmologist, Mount Sinai Hospital, New York. S. Refsum, a Norwegian physician.